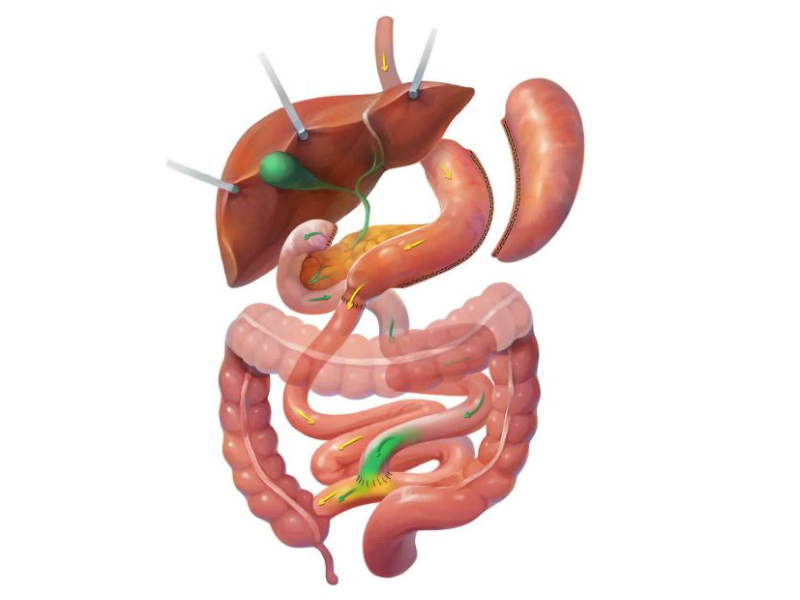
The duodenal switch (DS) or biliopancreatic diversion with duodenal switch is a tried-and-true metabolic surgery with a few decades of history.
However, the DS has only recently regained popularity as a surgical option for patients with severe morbid obesity – those with a BMI over 45 or 50. When it was first performed in the late 1980s, we knew far less about abdominal anatomy than we do today. As such, patients undergoing the DS often had significant gastrointestinal issues, including flatulence, foul-smelling stool, and diarrhea.
The DS soon brought about a new standalone procedure. In 2012, the first part of the DS, known as the gastric sleeve or sleeve gastrectomy, was approved by CMS as a covered standalone procedure. Before then, extremely obese patients would undergo the DS as a two-stage procedure, the first of which was a gastric sleeve, followed by the intestinal bypass. However, many patients with relatively lower BMI – those between 35 and 45 – did well with the sleeve alone.
Today, with standardization in technique and technology, the DS has become a more prevalent surgery because of its exceptional effectiveness and the fact that we’ve reduced many of the symptoms and side effects associated with it.