You may have heard of a dual procedure, single anesthesia surgery, where a friend or family member had their gallbladder removed at the same time as their bariatric procedure. You may be wondering if the same will happen during your bariatric surgery. Of course, it depends.
One of the most significant risks of gallstones and consequent gallbladder disease is obesity, and many obese patients also experience gallbladder problems. Some will already have had their gallbladder removed, while others may be experiencing gallbladder pain at the time of their surgical procedure.
It’s important to understand that gallstones do not go away, regardless of your future diet or any online hacks you may have seen. They are hard stone-like objects that can vary in size. So, once you have your first gallstone attack, they typically get more frequent and intense. To that end, gallbladder removal, known as a cholecystectomy, is the only option for getting permanent relief.
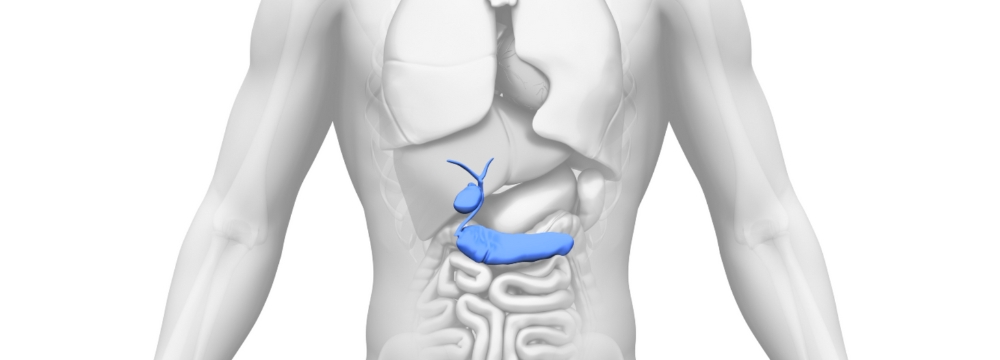
You’ll notice that the gallbladder is attached to the liver, and the liver partially occludes the stomach. This is one of the reasons why we use a liver retraction device during bariatric surgery. This keeps the liver away from the surgical field and allows us to perform the bariatric procedure without impediment. As such, we can also easily access the gallbladder, and it makes sense if patients suffer from gallstone attacks to address two concerns in one.
Will Gallbladder Removal Affect the Outcome of Bariatric Surgery?
The short answer is no; the gallbladder does not serve a vital purpose and can be removed easily without long-term postoperative concerns, especially regarding bariatric surgery. The recovery looks the same when compared to a bariatric-only procedure. Dr. Tsuda will guide you on potential gastrointestinal issues you may experience due to gallbladder removal and the loss of on-demand bile. Of course, with your lessened caloric intake after bariatric surgery and plenty of time for your liver to adapt, you should not experience any long-term GI concerns.
When We Don’t Remove the Gallbladder
Many patients understand that rapidly losing weight is another significant potential risk factor for gallstone formation. This happens because as we diet (and typically, our intake of high-fat foods decreases), the bile in the gallbladder accumulates and is not free-flowing. The bile can begin to crystallize and form stones. While this is the case after bariatric surgery, and some patients will go on to develop gallstones, prophylactic cholecystectomy is not appropriate. This is primarily because, with good postoperative hydration, proper diet, and regular exercise, most patients will not develop gallstones in the first place. Further, not all gallstones are symptomatic and a significant number of people, bariatric surgery or not, live their entire lives with gallstones without ever having an attack.
The Bottom Line
When you come into your consultation for bariatric surgery, you can speak to Dr. Tsuda about the possibility of a dual procedure if you are experiencing gallbladder issues. There is typically no added risk to removing the gallbladder, and there are no additional postoperative limitations past what you would have for bariatric surgery alone.
Ultimately, we aim to handle any abdominal issues as effectively as possible with the lowest risk. This can include removing your gallbladder if you have symptomatic gallstones or gallbladder disease. Whether you are considering bariatric surgery or wish to be evaluated for gallbladder issues, we encourage you to contact our office and schedule a consultation with Dr. Tsuda.